Key points
- Do not routinely image patients to diagnose Pediatric Mild Traumatic Brain Injury (mTBI).
- Use validated, age-appropriate symptom scales to diagnose mTBI.
- Assess evidence-based risk factors for prolonged recovery.
- Provide patients with instructions on return to activity customized to their symptoms.
- Counsel patients to return gradually to non-sports activities after no more than 1 to 2 days of rest.
Guiding principles
HEADS UP Training

Take action to improve the care of children with mTBI
The goal of the CDC Pediatric mTBI Guideline is to help healthcare providers take action to improve the health of their patients. The CDC Pediatric mTBI Guideline consists of 19 sets of clinical recommendations that cover diagnosis, prognosis, and management and treatment. These recommendations are for healthcare providers working in: inpatient, emergency, primary, and outpatient care settings.
The CDC Pediatric mTBI Guideline was developed through a rigorous process guided by the American Academy of Neurology and 2010 National Academy of Sciences methodologies. An extensive review of scientific literature, spanning 25 years of research, formed the basis of the Guideline.
Overview
- Read the Guideline
- Read the Systematic Review (that summarizes the evidence that forms the basis of the CDC Pediatric mTBI Guideline)
- Learn about validated symptom assessment tools and scales
Key Recommendations from the CDC Pediatric mTBI Guideline:
1. Do not routinely image patients to diagnose mTBI.
2. Use validated, age-appropriate symptom scales to diagnose mTBI.
3. Assess evidence-based risk factors for prolonged recovery.
4. Provide patients with instructions on return to activity customized to their symptoms.
5. Counsel patients to return gradually to non-sports activities after no more than 1 to 2 days of rest.
Resources
Provider Tools
Checklist on Diagnosis and Management
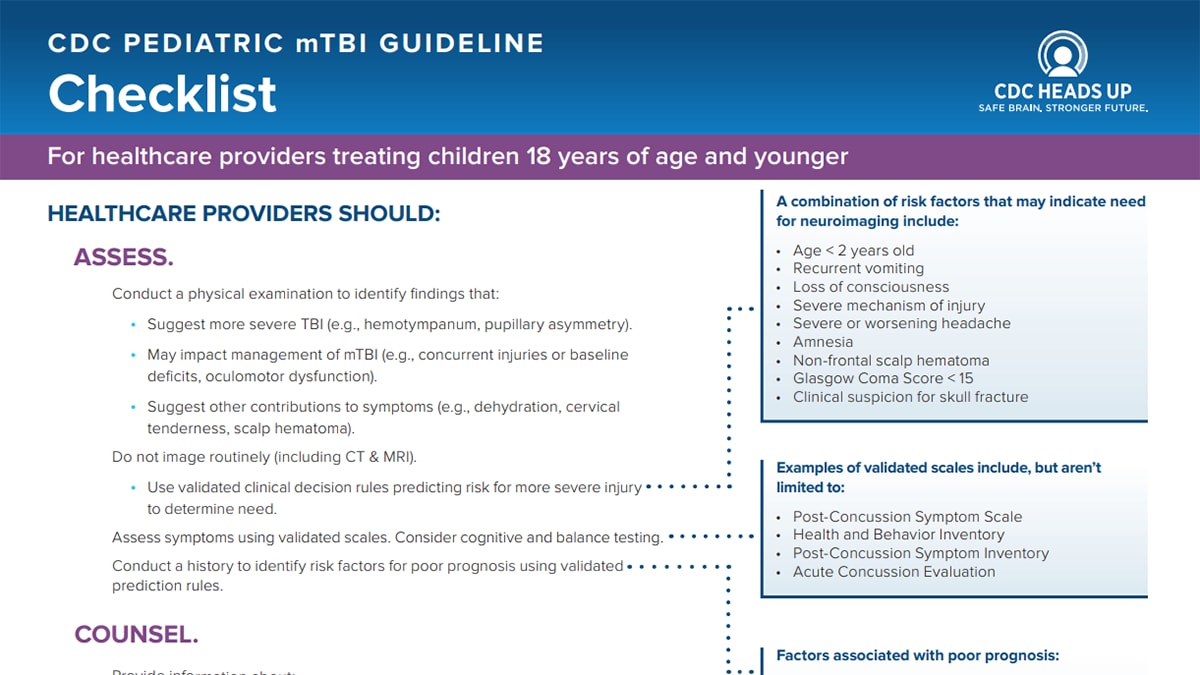
Download: Checklist on Diagnosis and Management
View Checklist on Diagnosis and Management as a Web Page
At A Glance: Prognosis
At A Glance: Diagnosis
At A Glance: Treatment
Letter to schools to be filled in by healthcare providers
Acute Concussion Evaluation (ACE) Forms
The ACE (Acute Concussion Evaluation) forms are patient assessment tools.
DOWNLOAD
Physician/Clinician office ACE form
Training
Click here for more information about the HEADS UP to Healthcare Providers online training.
Patient and Family Resources
Discharge Instructions
Symptom-based Recovery Tips
To learn more about concussion, such as the signs and symptoms and how to safely return to school and sports after a concussion, check out the CDC HEADS UP website.